Index
THEretinal vein occlusion (RVO, from English Rethinal Va Occlusion) is an eye disease caused by the obstruction of a venous vessel of the retina.
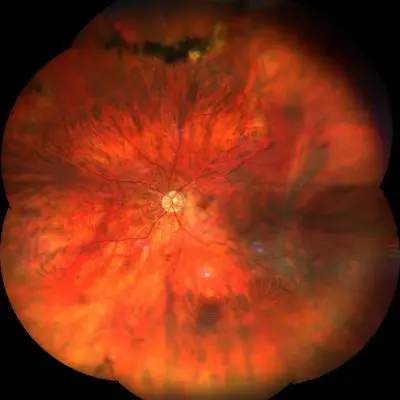
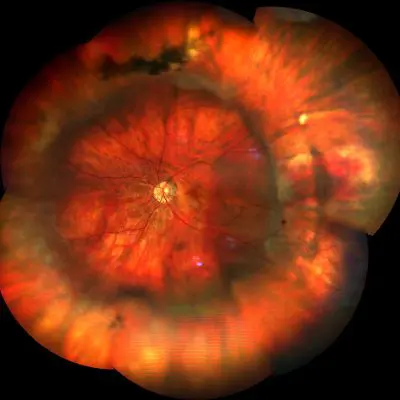
Based on the vascular district involved, retinal vein occlusion can be distinguished into occlusion of the central retinal vein (CRV extension, from English Ccentral Rethinal Va Occlusion) and occlusion of a branch of the retinal vein (BRVO extension, from English Branch Rethinal Va Occlusion). The first is caused by the obstruction of the main retinal vein, the second by the obstruction of one of its branches.
Some people have one predisposition - that is a higher risk - for retinal vein occlusion due to the existence of a particular anatomical conformation of the blood vessels of the retina. Even the diabetes, glaucoma,hypertension, age-related vascular pathologies and some blood disorders represent a risk factor for RVO. In addition, a previous event of BRVO in one eye leads to a greater probability (by approximately 10%) that a second event of BRVO or CRVO may occur in the other eye within 5 years of the initial thrombotic episode.
Symptoms and Diagnosis
The symptoms most commonly reported by patients affected by retinal vein occlusion are the perception of blurry images and the more or less serious and sudden lowering of both central and peripheral vision.
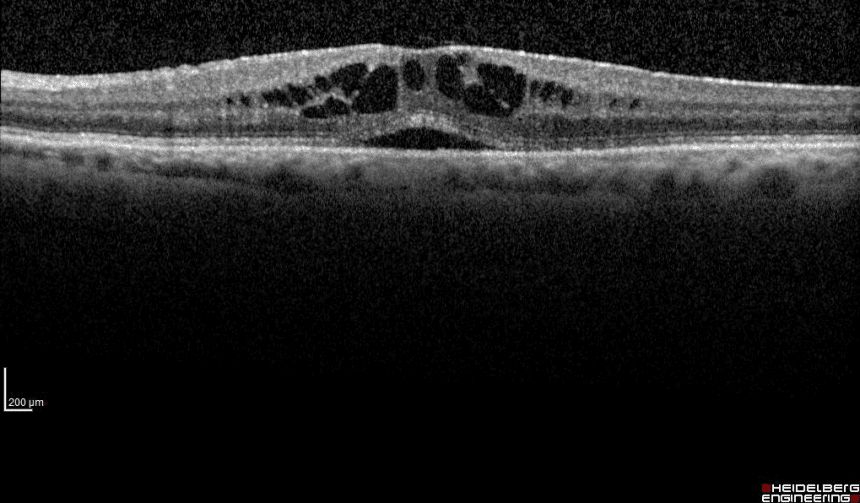
Retinal vein occlusion is diagnosed already in the early stages of the eye examination through theophthalmoscopy and then, in a more precise and in-depth way, by means of some instrumental tests such as the Optical Coherence Tomography (OCT) high resolution, which allows you to view each individual retinal layer, and theFluorescein angiography (FAG), which allows to examine the structural integrity and patency of the blood vessels of the retina with the use of a contrast medium.
Complications of retinal vein occusion
Retinal vein occlusion can give rise to different types of complications such asvitreous hemorrhage,post-thrombotic cystoid macular edema, neovascularization pathological , iris neovascularization which, in turn, can generate the neovascular glaucoma.
Let's look at some complications below.
Vitreous hemorrhage
Vitreous hemorrhage occurs when a capillary in the retina breaks and blood permeates the vitreous body. This type of event leads to an immediate loss of vision as the presence of blood prevents light from passing through the hemorrhagic vitreous (hemovitreus). Sometimes the vitreous hemorrhage reabsorbs spontaneously, sometimes it can take many weeks or a few months before the patient returns to see.
When the hemorrhage is not reabsorbed spontaneously within a reasonable time (6-8 weeks) or if the presence of blood represents a danger to the health of the retina, surgery called vitrectomy is used, which consists in the removal of the blood vitreous and its replacement with a suitable medium, usually a gas or a balanced salt solution (BSS), which will then be replaced by a "second formation" vitreous.
Post-thrombotic cystoid macular edema
Cystoid macular edema (CM extension, from English Cystoid Macular EPost-thrombotic dema) occurs when blood and fluid from a blocked or damaged retinal blood vessel accumulates under the retina, causing the macula to lift.
This phenomenon causes blurry vision and in the absence of timely treatment can lead to an important and irreversible reduction of central vision. CME must be treated with intravitreal injections of anti-VEGF drugs (anti Vascular Endothelial GRowth Factor), which inhibit the pathological effect of VEGF produced in excess by ischemic retinal areas.
Pathological neovascularization
Pathological neovascularization consists in the growth of new fragile and diseased blood vessels. In the case of retinal vein occlusion, this phenomenon can occur in the retina or iris and can lead to a blockage of the drainage channels of the aqueous humor, with increased intraocular pressure and consequent neovascular glaucoma, a pathological entity that is particularly difficult to treat.
Prevention of retinal vein occlusion
If retinal vein occlusion is not diagnosed and treated urgently, the onset of various complications can lead to irreversible vision loss. There prevention remains undoubtedly the most effective weapon against RVO and consists in keeping correlated risk factors under control, such as diabetes,hypertension,hypercholesterolemia, glaucoma, smoke.
Treatment of retinal vein occlusion
complicated by post-thrombotic cystoid macular edemaTherapy for retinal vein occlusion complicated by post-thrombotic cystoid macular edema is characterized by two different phases. The first phase consists in the treatment of the peripheral ischemic retinal areas, previously identified during fluorescein angiography, by means of a duplicate frequency laser (DDF).
The second phase involves the treatment of cystoid macular edema secondary to venous occlusion with intravitreal injections of anti-VEGF drugs, which aim to prevent or combat the pathological effect of VEGF produced in excess by ischemic retinal areas. A few days after intraocular administration of anti-VEGF drugs, the macula tends to return to its normal anatomical and physiological shape, furthermore the patient's initial visual capacity is restored or significantly improved.
Slow-release intravitreal implants are also used to counteract the pathological action of VEGF, biodegradable polymers based on cortisone molecules which are implanted into the vitreous cavity, where they release pharmacologically active molecules in a controlled manner for several months or even years.
Pathology and treatment on video
Do you need more information?
Do not hesitate to contact me for any doubt or clarification. I will evaluate your problem and it will be my concern and that of my staff to answer you as quickly as possible.