Although cataract removal surgery is one of the safest and most performed procedures today, some patients may not achieve the excellent postoperative results expected for developing a complication called cystoid macular edema (CME).
CME was first reported by Irvine in 1953 and angiographically demonstrated by Gass and Norton in 1966, thus taking the name of Irvine-Gass Syndrome. Normally CME appears within 4 months of cataract surgery in acute form, if it occurs after 4 months it is considered late onset, if it lasts more than 6 months it is classified as chronic.
This unwanted complication can also occur following uncomplicated surgeries but in particular with the coexistence of other ocular pathologies, in complicated surgeries or in patients suffering from uveitis or diabetic retinopathy.
Over the years, the continuous evolution of surgical techniques has made this intervention minimally invasive, significantly reducing the incidence of CME. Nevertheless, still today, numerous factors contribute to its development following cataract surgery: the toxicity of light, the presence of a macular vitreous traction, inflammatory mediators, the use of adrenergic drugs, age, vitreous loss , the integrity of the posterior capsule, hypertension and diabetes.
Below we briefly analyze these factors.
Although it was originally assumed that the light from the operating microscope had some toxicity and could contribute to CME, a prospective randomized study did not actually support this hypothesis.
Age is another factor that must be considered primarily, as there is certainly a positive correlation between the increase in patient years and an increase in the incidence of CME.
The changes that occur in the vitreous body during surgery are another potential pathogenic mechanism, since vitreous loss during surgery has been shown to increase the prevalence of CME by 10-20%.
Iris incarceration, iris trauma, rupture of the posterior lens capsule, displacement of the intraocular lens (IOL) and the persistence of residual fragments of the natural lens inside the eye represent complications capable of inducing a possible appearance of CME. .
There is also an increase in the incidence of CME associated with prostaglandins determined by an increase in the breakdown of the blood-aqueous barrier and inflammatory activity.
Ultimately, inflammation is considered the major risk factor in the development of a post-operative CME. It is likely that after surgery, inflammatory mediators (prostaglandins, cytokines and other vascular permeability factors) are released from the anterior segment of the eye and diffused through the vitreous cavity to the retina, stimulating the breakdown of the blood-borne barrier (Blood -Retinal Barrier, BRB) and the subsequent leakage of liquids through the walls of the retinal vessels and the retinal pigment epithelium (RPE) in the perifoveal retinal tissues with consequent development of macular edema.
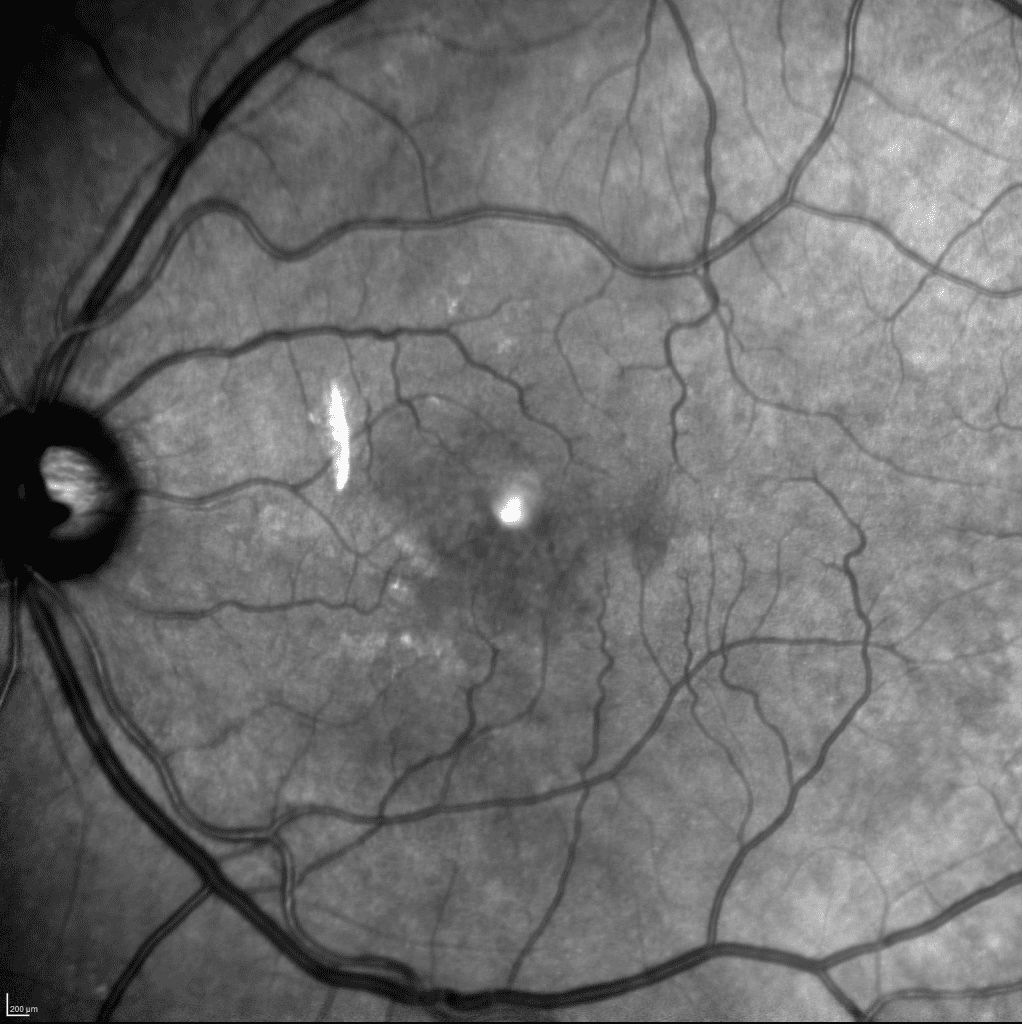
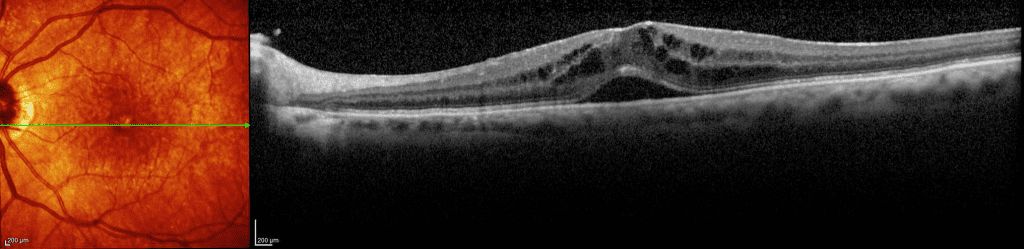
CME is diagnosed with biomicroscopy, optical coherence tomography (OCT), or fluorescence angiography (AF). It is characterized by the presence of cystic spaces in the outer nuclear layer with yellowish coloring in the perifoveal area and the disappearance of the physiological foveal depression with retinal thickening. In the initial stages of AF, capillary dilatation, leakage from the perifoveal capillaries and hyperfluorescence of the macula and optic disc are highlighted, in the late stages a “flower petal” pattern is reached.
In severe CME, the cystic spaces, which extend outside the perifoveal region, may have a “honeycomb” appearance in AF proportional to their extent and consistency.
As a precaution, in patients potentially at risk, the use of non-steroidal anti-inflammatory drugs (NSAIDs) is recommended before surgery and the combination of steroids and NSAIDs in the postoperative period to reduce the incidence of CME.
In 90% of patients with macular edema arising after cataract surgery there is already a spontaneous resolution in a few weeks with restoration of visual acuity.
In the absence of it, the prescription of topical corticosteroids and non-steroidal anti-inflammatory agents can help with its resolution, which can sometimes last up to 6 months, by blocking the release of inflammatory mediators in the anterior segment.
Corticosteroids are very effective, but since in some “sensitive” patients they lead to a rise in intraocular pressure (IOP) they should be used with particular caution and monitoring IOP at least every 2 weeks.
In the event that the patient does not respond to topical therapy, he will have to be subjected to intravitreal injections of anti-VEGF (Vascular Endothelial Growth Factor), molecules that act on the endothelial cells of the vessels reducing vascular permeability and inhibiting VEGF, or to a implantation with slow-release corticosteroids that increase the activation of anti-inflammatory genes, reducing the synthesis of VEGF and inhibiting vascular permeability.
In patients in whom an incarceration of the vitreous has occurred during cataract surgery, vitreolysis with the YAG laser has shown extremely positive effects, especially with the latest generation lasers that emit radiant energy with pulses in the order of billionths of a seconds. In some patients, particularly refractory to pharmacological or laser therapies applied, it may be necessary to perform a vitrectomy surgery that allows to gently and completely remove the otherwise unreachable vitreous adhesions and the inflammatory mediators themselves allowing at the same time and better access of topical drugs to the posterior pole.
Today, a variety of therapeutic means exist to treat and resolve cystoid macular edema (CME). An essential condition for achieving therapeutic success is that diagnosis is early and that all currently available therapies, diversified from patient to patient, are considered as part of a "personalized medicine" applied to ophthalmology.

