Promising results in LHON's phase three gene therapy study
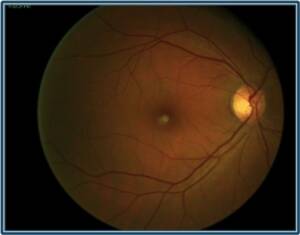
Leber's hereditary optic neuropathy (LHON) is a maternally transmitted mitochondrial neurodegenerative disease of the optic nerve.
It is the most common mitochondrial DNA (mtDNA) disease affecting approximately 1 in 30.000 to 1 in 50.000 people, particularly young adult males. The pathophysiology of LHON is characterized by the selective loss of retinal ganglion cells (RGC) and their axons, leading to progressive and rapid bilateral vision loss. Visual prognosis is poor and most patients have 20/200 visual decay within the first year of disease onset.
Leber Hereditary Optic Neuropathy
Contents Leber's hereditary optic neuropathy (Leber Hereditary Optic Neuropathy - LHON) is a very rare mitochondrial disease affecting the ganglion cells of the optic nerve. Manifests
REVERSE is a randomized, double-blind, multicentre Phase 3 clinical trial that evaluated the efficacy of a single intravitreal injection of rAAV2 / 2-ND4 in subjects with Leber Hereditary Optic Neuropathy (LHON) vision loss.
RAAV2 / 2-ND4 (GS010) is a recombinant replication defect adeno-associated virus, serotype 2, which contains a modified cDNA encoding the human mitochondrial wild-type protein ND4 and a specific MTS for protein translocation in the mitochondrial matrix.
A total of 37 carriers of the mutation m.11778G> A (MT-ND4) and with duration of vision loss ranging from 6 to 12 months were treated. Each subject's right eye was randomly assigned to treatment with rAAV2 / 2-ND4 (GS010) or placebo injection. The left eye received treatment not assigned to the right eye.
Unexpectedly, sustained visual improvement was observed in both eyes during the 96-week follow-up period. At the end of the period, eyes treated with rAAV2 / 2-ND4 showed a mean improvement in visual acuity corrected (BCVA) of -0,308 LogMAR (+15 letters ETDRS). A mean improvement of -0,259 LogMAR (+13 ETDRS letters) was observed in eyes treated with placebo.
At week 96, 25 subjects (68%) had clinically relevant BCVA recovery from baseline in at least one eye and 29 subjects (78%) had improved vision in both eyes.
It is hypothesized that the positive effects produced by the treatment, even in the contralateral eye, are attributable to the inter-eye transfer of the viral vector rAAV2 / 2-ND4.
In a rodent study, a tracer dye injected intravitreally into the rat's eye was detected in the optic nerves of the contralateral non-injected eyes: this suggests that there is an axonal or glial transfer through the anterior visual pathways. There is also evidence to support transneuronal spread, possibly through synaptic transfer mechanisms.
It has been shown that mitochondria can migrate long distances into axons to distribute energy and allow distal neuronal activity, in fact, mitochondria within RGC axons can also be engulfed in vesicles and exported to astrocytes found at high density in the optic nerve head and then stored in the endosomes.
The dense network of interconnected astrocytic processes could, therefore, allow cell-to-cell long-distance transfer of cytoplasmic elements via membrane junctions. Another hypothetical mechanism underlying the contralateral improvement is brain plasticity with reorganization of the visual areas contributing to the visual improvement of the contralateral non-injected eyes.
The therapy aims to save retinal ganglion cells from the mutation caused by LHON by replacing the defective gene.
This important step is added to the gene therapies recently introduced in the treatment of other severe and disabling forms of hereditary-familial retinal pathologies.
Note to the reader:
When a study is in phase three: it has come to the point of understanding how effective the drug is, if it has any more benefits than similar drugs already on the market and what is the relationship between risk and benefit. In this phase, to validate the efficacy of the study, the patients "enrolled" are hundreds or thousands.

