Index
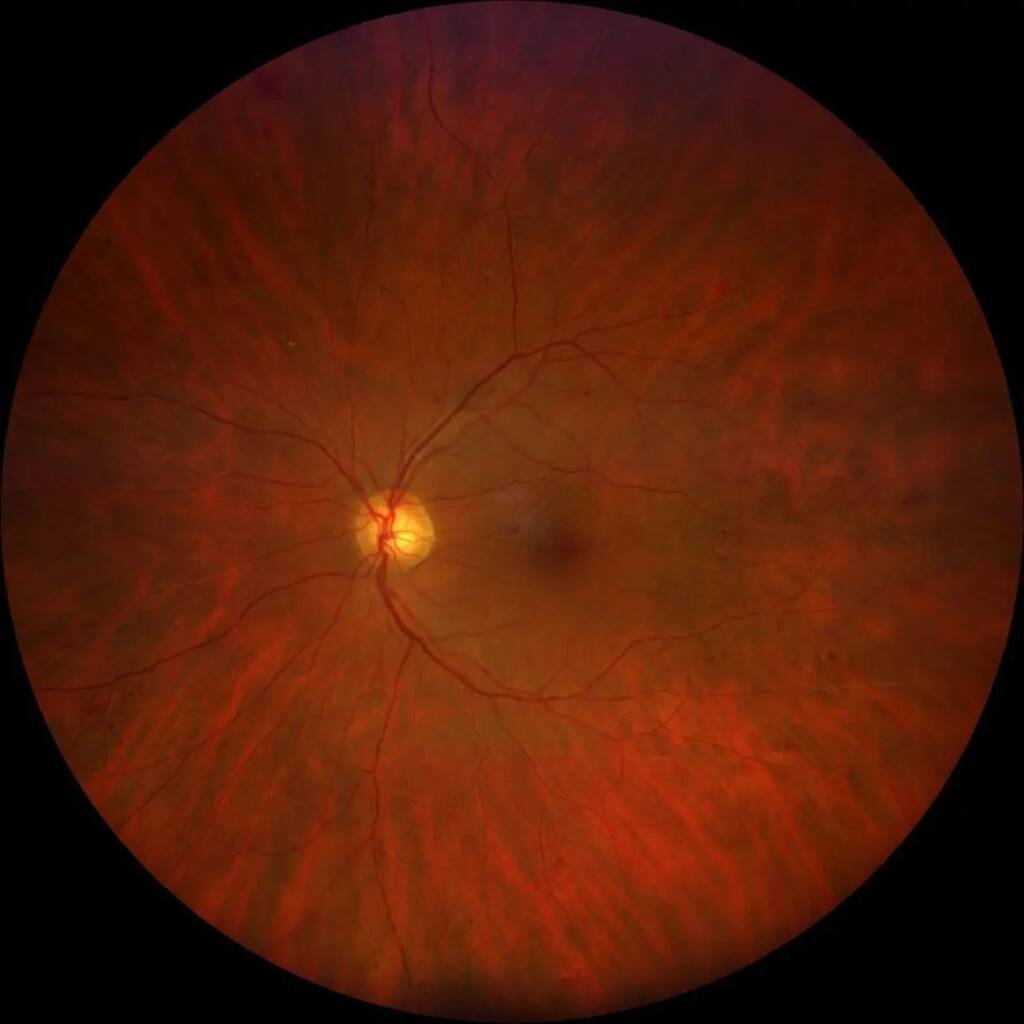
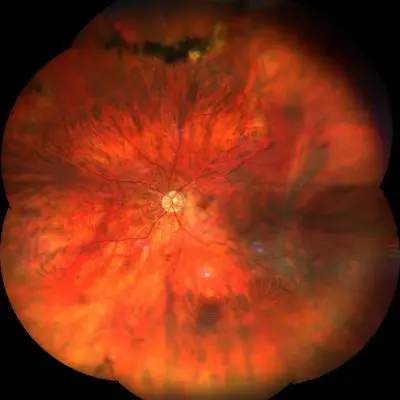
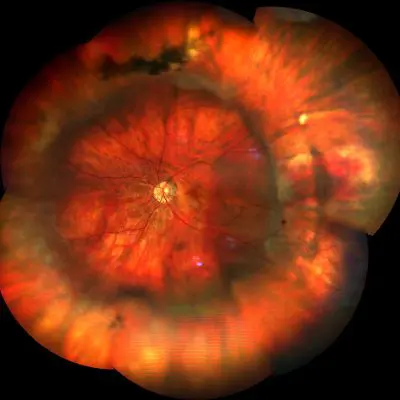
Non-proliferative diabetic retinopathy (NPDR) is classified into mild, moderate, severe and very severe
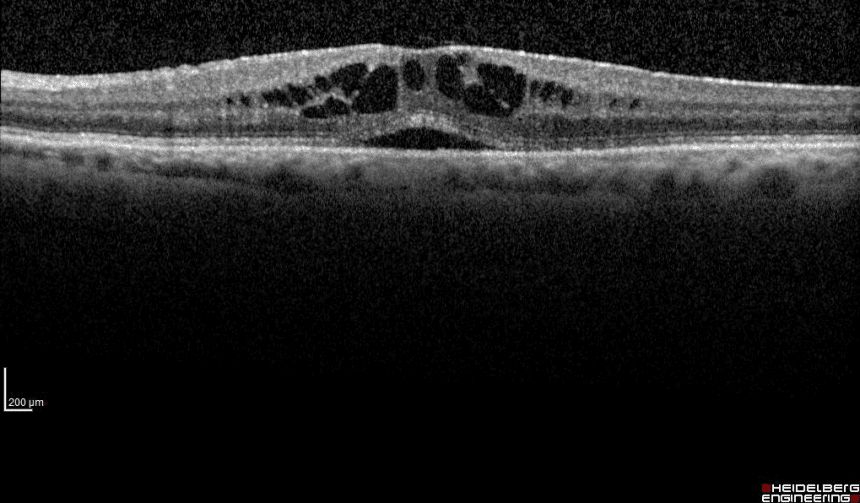
It is characterized by the presence of infarcts of the nerve fiber layer (cottony exudates), retinal vascular abnormalities including venous dilation, retinal microaneurysms, intraretinal microvascular abnormalities, areas of capillary non-perfusion, retinal hemorrhages, hard exudates (leakage of lipid and protein material) and macular edema.
Non-proliferative diabetic retinopathy it is characterized by the presence of microaneurysms (hypercellular extroversions of retinal capillaries with weakened walls due to the loss of pericytes) saccular capillaries, capillaries lacking in pericytes, and acellular or eliminated capillaries. The loss of pericytes is evidenced by an excessive number of "ghost" pericytes on the capillaries, the phantom creates a pocket in the basement membrane that was formally occupied by the pericyte.
The apparently functioning acellular capillaries degenerated to remain only a basement membrane tube. Acellular and degenerated capillaries are not perfused and can be filled with cytoplasmic processes of glial cells.
Capillary occlusion occurs initially in a single capillary isolate and has no clinical consequences in the early stages. Cell death and increased capillary permeability can be followed by cycles of renewal and further cell death, leading to progressive microvascular loss and ischemia resulting in the release of vasoproliferative factors (such as VEGF, erythroproteins and others) in the ischemic retinal areas.
Vascular endothelial growth factor (VEGF) is secreted by the ischemic retina. VEGF leads to an increase in vascular permeability with consequent edema of the retina and to angiogenesis, new blood vessel formation.
Diagnosis
Most patients do not present with symptoms, except when they are in the late stages of the disease. Diabetic retinopathy can seriously and irreversibly impair vision. THE main symptoms of this pathology are: blurring of central vision, difficulty in the perception of colors and sometimes reduction of night vision.
Available treatments are generally effective in preserving vision, but unfortunately they are not definitive, as patients often require periodic retreatment.
The most effective weapon against this dangerous pathology remains prevention, obtained mainly through strict blood sugar control and early diagnosis, implemented thanks to careful and regular monitoring of the retina through tests such as: Optical Coherence Tomography (OCT) high resolution to examine every single retinal layer and identify the presence of a cystoid macular edema; L'Fluorescence Angiography with Fluorescein (FAG) andIndocyanine Green Angiography (ICGA), minimally invasive tests performed with two contrast media, essential for the identification of ischemic areas in the peripheral retina and any associated neovascular membranes.
These tests make it possible to diagnose diabetic retinopathy early and, if necessary, to intervene promptly with the most appropriate treatment before major damage to vision arises.
Diabetic patients should follow a prevention protocol associated with regular retinal monitoring within the first year of diabetes diagnosis. Diabetic pregnant women must undergo particularly careful checks as early as the first trimester, as diabetic retinopathy can progress very rapidly during gestation.
Treatment
Pathology and treatment on video
Do you need more information?
Do not hesitate to contact me for any doubt or clarification. I will evaluate your problem and it will be my concern and that of my staff to answer you as quickly as possible.