Index
Exudative maculopathy (Wet AMD) or the age-related macular degeneration of the neovascular type (Neovascular Age-related Macular Degeneration, nAMD) is a serious eye disease that affects the macula, that is the portion of the central retina responsible for the vision fine and detailed that allows us to recognize a face, read, perform precision work, drive the car ..
In technologically advanced countries, the incidence of AMD has increased strongly and continues to increase due primarily to the increase in the average life span and the concomitance of numerous other environmental and nutritional factors in addition to the sometimes predominant genetic ones. In fact, AMD affects about 11% of people between the ages of 65 and 74 and this percentage increases significantly as older age groups are considered. Today, AMD is the most common cause of legal blindness and low vision in people over the age of 55.
AMD can come in two forms:Atrophic AMD (o non-neovascular o shoal) and theWet AMD (o neovascular o humid). AMD usually begins in the atrophic form (90% of cases) and more rarely (10% of cases) in the exudative form. In some patients, atrophic AMD can evolve into an exudative form.
Exudative maculopathy is caused by the uncontrolled growth of pathological new vessels under the retina, a process known as pathological neoangiogenesis.
The "normal" (healthy) physiological process that leads to the formation of new blood vessels in the body (essential during growth, wound healing or pregnancy) is known as angiogenesis; in the case of AMD, however, the newly formed blood vessels are defective, diseased, and for this reason we speak of pathological neoangiogenesis and pathological new vessels.
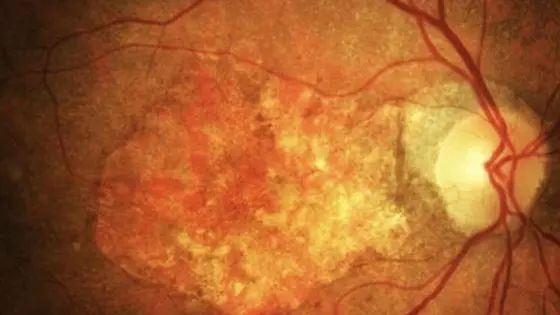
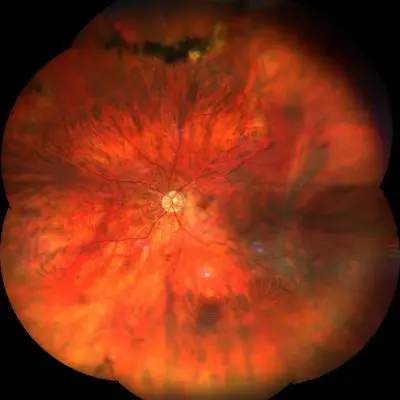
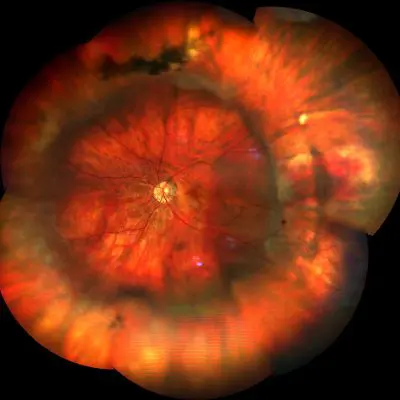
These tend to lose blood and fluids under the retina and result in the lifting of the macula from its original position, thus causing damage to the retinal pigment epithelium (RPE) and photoreceptors which, if they remain separated from their source of oxygen and nourishment for a long time, undergo cell death. The death of macular photoreceptors determines the loss of central vision, with the appearance of a dark spot or blind spot in the center of the vision. In the presence of bleeding below the macula, scar tissue can form which can lead to irreversible loss of central vision in a relatively short time.
Pathological neoangiogenesis is caused by physiological events resulting from the aging process of the cells and tissues of the eye, such as the formation of confluent drusen, oxidative stress and hypoxia.
Le friendly are tiny accumulations of waste material resulting from the metabolism of retinal cells, they form under the retina - between theretinal pigment epithelium (EPR) and the Bruch's membrane - and appear as small yellowish spots visible on fundus and eye examination retinography. Over time, drusen tend to increase in number and size until they merge with each other and form larger piles of waste material known as confluent drusen.
Lo oxidative stress it is a condition of great imbalance of the cells, which can cause their malfunction or death. Oxidative stress is caused by the presence of excessive quantities of highly reactive molecules, including i free radicals. Many of these molecules are formed daily inside cells such as by-products of metabolism or by the action of UV rays (photoxidation) or enter the cells through thesupply (free radicals are abundant in foods cooked at very high temperatures). Usually, reactive species and free radicals are neutralized or eliminated by cells, but as we age, some cell functions become less efficient and this can lead to more production and / or less disposal of these molecules, which in this way they accumulate in cells and tissues. It is very important to underline that the increased presence of UV rays in the atmosphere - due to the ozone hole - is one of the main causes of the formation of free radicals in the retina, since UV rays also arrive directly on the retina.
hypoxia it means a state of low oxygen supply to a tissue. In the eye, aging can lead to a thickening of Bruch's membrane, which can decrease or prevent the passage of oxygen and nutrients from the blood vessels of the choroid to the macula. Similarly, the increase in thickness of Bruch's membrane represents an obstacle to the removal of retinal catabolites. The presence of confluent drusen - characteristic of the advanced stage of atrophic AMD - causes further separation of the retina from the vascular layer and therefore contributes to the onset of a condition of hypoxia.
The presence of confluent drusen, oxidative stress and hypoxia in the retina can give rise to a process ofinflammation during which particular named molecules are released endothelial growth factors, which stimulate the fformation of new blood vessels. The main growth factor identified and involved in the onset of wet AMD is the vascular endothelial growth factor (VEGF), which spreads within the choroid and stimulates the growth of new pathological blood vessels.
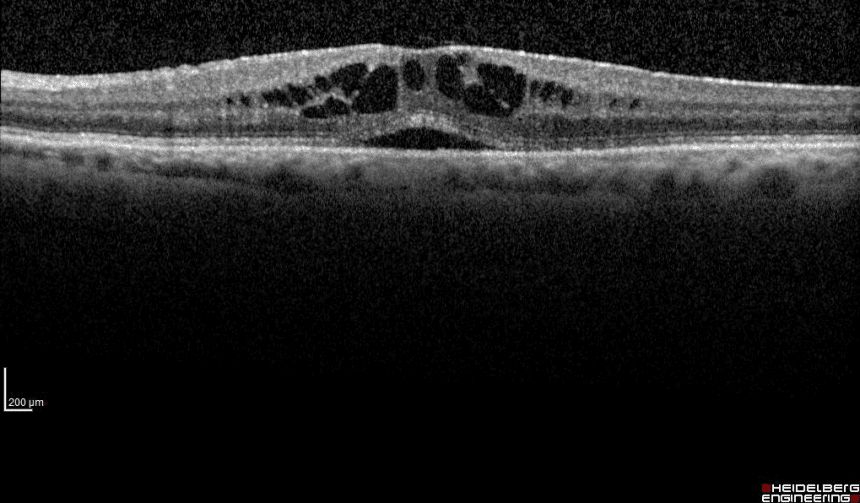
The formation of pathological new vessels marks theonset of exudative maculopathy. Pathological new vessels grow from the choroid and choriocapillary, penetrate through Bruch's membrane and proliferate further in the subretinal space, to form a structure known as choroidal neovascular membrane (CNV), from which there is a leakage of fluids and blood that accumulate under the macula. The accumulation of fluids in this point seriously and rapidly compromises the anatomical structure and macular function, which being removed from its physiological position, is separated from its source of oxygen and nourishment. Prolonged lack of oxygen and nutrients causes macular cell death and consequent loss of central vision. Loss of central vision can also occur due to the formation of scar tissue on the macula.
4 Types of exudative maculopathy
- Type 1 o Occult CNV: develops below the RPE retinal pigment epithelium. It is diagnosed only thanks to theindocyanine green angiography and sometimes in the most severe forms it presents with retinal hemorrhages. The patient perceives a whole image, but with distortions.
- Type 2 o Classic CNV: it develops above the EPR retinal pigment epithelium. It can be diagnosed either with high definition Optical Coherence Tomography (OCT) or with Fluorescence Angiography (FAG) or Indocyanine Green (ICGA); this is usually the most severe form because it develops large scars from which central vision is lost.
- Type 3 o polypoid vasculopathy (IPVC): it develops below the retinal pigment epithelium, but has a circumscribed and well-defined pseudopoidal shape.
- Type 4 o retinal angiomatous proliferation (RAP): it develops inside the retina and proliferates downwards creating an anastomosis, that is a pathological communication directly between the retinal artery and a vein of the choriocapillary. These are usually the forms that best respond to intravitreal therapy with anti-VEGF.
Symptoms
Patients suffering from exudative maculopathy perceive symptoms such as distortion of images, wavy perception of lines, the presence of a scotoma in the center of the vision which can arise suddenly and immediately become very serious. The evolution of the pathology can become extremely rapid and dramatic in the presence of hemorrhage at the level of the vascular membrane: in these cases the loss of central vision can occur even in a few seconds.
For the above reasons, it becomes evident that the prevention of exudative maculopathy is of fundamental importance to avoid or at least limit the damage deriving from this serious ocular pathology. Prevention is important for all people over the age of 50 and is essential for patients with atrophic AMD, in whom the risk of evolving into wet AMD is always present.
Diagnosis
Treatment
Treatment for wet AMD involves a series of intravitreal injections of anti-VEGF drugs. Although this procedure is effective in preventing or delaying the loss of central vision, it should be borne in mind that to date there is no definitive treatment for wet AMD and therefore prevention is a particularly effective weapon to defend against this serious pathology. retinal.
The inflammatory process that causes the onset of wet AMD involves a series of biochemical reactions known as complement cascade; this can be modulated thanks to a named factor CFH factor. The CFH factor regulates the extent of the inflammatory response, which in healthy people increases or decreases as needed; some variants of the gene that codes for the CFH factor are related to the inability of the CFH factor to modulate - in particular to "brake" and control - the inflammatory response, therefore in subjects in which there is the presence of one of these variants genetics of the CFH factor, there is an increased risk of developing AMD (genetic susceptibility).
Since the identified variants of the CFH gene responsible for the genetic susceptibility for AMD are different, several are available genetic testing that allow to highlight its presence. The test is especially recommended for people who are familiar with wet, but also atrophic AMD. Presenting genetic susceptibility for AMD does not mean being destined to get sick, but on the contrary, this information allows the adoption of prevention protocols capable of reducing the risk of onset of this pathology. Prevention protocols are based on the adoption of very healthy lifestyles, which exclude as much as possible the presence of environmental and behavioral risk factors. For genetic testing to be of help, it must be rigorously performed and interpreted by experienced geneticists.
Pathology and treatment on video
Do you need more information?
Do not hesitate to contact me for any doubt or clarification. I will evaluate your problem and it will be my concern and that of my staff to answer you as quickly as possible.