Index
Il retinal detachment it is an extremely dangerous event for the vision and represents a real one eye emergency.
Under normal conditions, the retina adheres to the fundus and receives oxygen and nutrition from the vascular network of the choroid through the cells of the retinal pigment epithelium.
When the retina detaches from the back of the eye, the photoreceptors present in the portion of tissue involved in the detachment lose contact with the retinal pigment epithelium and are deprived of the nourishment and oxygen they need.
In this circumstance, cones and rods are no longer able to perform their function correctly and an important visual impairment. If action is not taken in an adequate and timely manner, the photoreceptors undergo cell death and the visual impairment turns into permanent loss of vision.
Cause of retinal detachment
Retinal detachment can occur as a result of a retinal tear or a macular hole, but also as a complication of proliferative diabetic retinopathy. In some cases, retinal detachment can be caused by a eye trauma.
After 40-45 years of age, the vitreous body undergoes chemical-physical transformations which determine its contraction and consequent detachment from the fundus of the eye. This phenomenon is common and usually resolves on its own without causing problems.
In some cases, however, the vitreous remains adhered to the retina pulling it towards the inside of the eye and if this traction lasts over time or becomes particularly intense, a retinal rupture can occur. When there is a retinal break, the vitreous infiltrates under the retina causing its detachment from the fundus and progressive detachment.
If, when it contracts, the vitreous remains attached to the macula, the central part of the retina, a condition known as vitreous-macular traction. Also in this case the problem can resolve itself, but if the traction persists over time, or increases, there may be the formation of a macular hole which, similar to what happens for retinal tears, can favor a detachment of the retina.
Symptoms
Among the symptoms of retinal detachment we can find
- flashes of light, caused by the formation of retinal tears;
- the sudden appearance of a large number of floaters, due to hemorrhage that can occur in conjunction with the retinal tear;
- shading in the peripheral visual field or the sensation of having a gray curtain passing in front of the vision, due to the flaps of detached retina that are in the optical path of light inside the eye.
These symptoms do not necessarily indicate that the retinal detachment has already occurred or is in progress, but they are certainly important symptoms that require urgent attention from an ophthalmologist as they could be a warning of a retinal detachment.
Diagnosis
In the presence of warning or suspicious symptoms, a thorough examination with examination of the ocular fundus must be performed, together with instrumental examinations capable of providing detailed information on the state of the retina and planning any surgery or para-surgery.
Among the most suitable instrumental tests we find
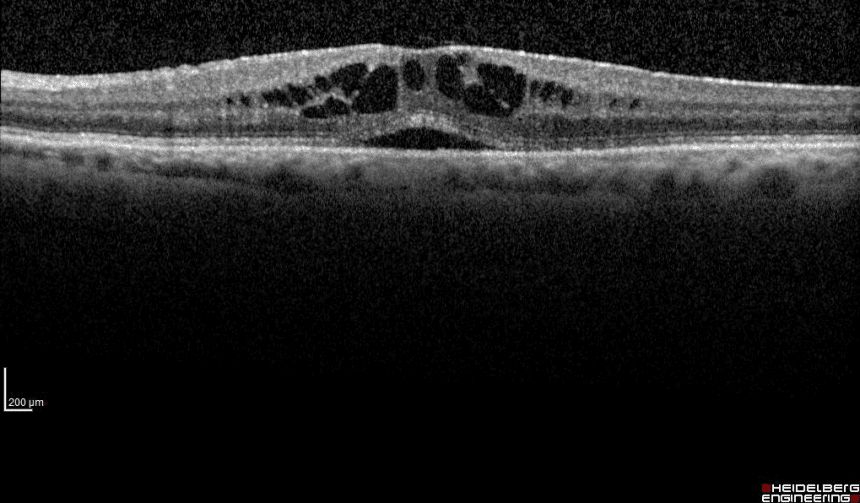
- la optical coherence tomography (OCT) high resolution, to analyze each individual retinal layer and quantify any infiltration of vitreous under the retina;
- theB-scan ultrasound, to evaluate any traction points of the vitreous on the retina;
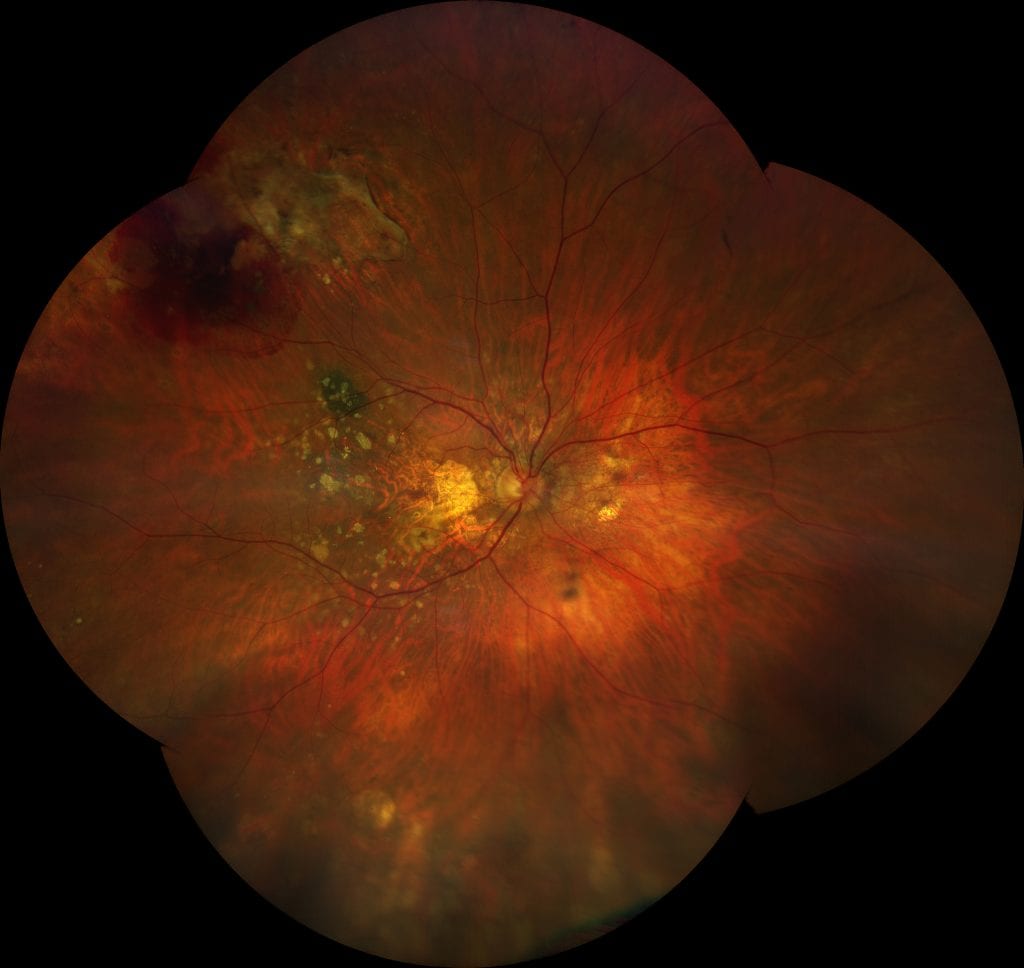
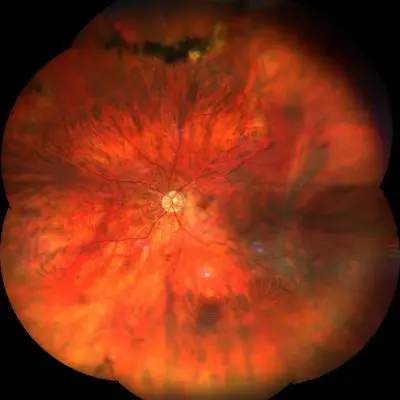
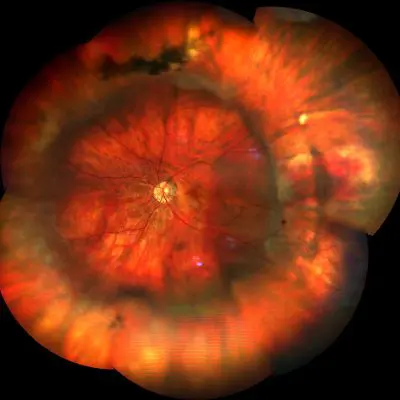
- la ultra wide field retinography, to document the presence of any peripheral retinal lesions and, if necessary, to decide whether to intervene through a para-surgical treatment, such as a laser, or through a real surgery, such as cerclage or vitrectomy.
Treatment
Retinal detachment should be treated promptly, even if only with initial and limited vitreous infiltration.
If the detachment is limited and clearly visible to the slit lamp, a para-surgical treatment with a photocoagulative laser. This treatment creates a “seal” around the affected retinal area in order to isolate the lesion.
In the event that the retinal detachment is very extensive, the patient must be immediately subjected to a cerclage and / or vitrectomy surgery. In most cases the latter is also the optimal option for not inducing post-operative refractive defects (myopia).
Il cerclage consists in applying a silicone band around the eyeball, more precisely on the sclera near the equator, to facilitate the re-attachment of the retina to the back of the eye. When cerclage alone fails to resolve the retinal detachment, a variant of the surgical technique can be practiced which also involves a plumbing, i.e. the insertion of additional silicone parts in correspondence with the retinal break to promote its closure.
Cerclage is the optimal option for young patients because, acting externally to the eyeball, it avoids the risk of inducing the early appearance of cataract, as would happen with vitrectomy.
La vitrectomy is a surgical intervention aimed at removing the vitreous, the cause of the traction that puts the retina at risk of forming a hole or a retinal break, or that caused it. If the retinal detachment has already occurred, the vitrectomy allows the retina to be repositioned in a short time on the ocular fundus, in order to prevent the photoreceptors from undergoing an irreversible degenerative process that leads to blindness.
Since retinal detachment is always a very dangerous event for vision, in the event of sudden onset of warning symptoms such as flashes and "flying flies" it is necessary to perform an eye check, especially in the presence of high myopia (and therefore of probable retinal degenerations), of a previous cataract surgery, of a retinal detachment that has already occurred in the other eye or of familiarity with this pathology.
Pathology and treatment on video
Answers to frequently asked questions
What are the symptoms of retinal detachment?
The symptoms caused by retinal detachment can be summarized as follows:
- vision of fixed black spots
- bright flashes (phosphenes)
- blurred vision especially if the central region (macula) is affected
- floaters (floaters)
- scotoma that covers part of the visual field like a dark curtain
What causes retinal detachment?
Retinal detachment is one of the main emergencies in ophthalmology. This condition is caused by the separation of the outer layer, the pigment epithelium, from the inner layer, the sensorineural retina.
How does a person with retinal detachment see?
A person with retinal detachment reports the appearance of:
- bright flashes
- perception of fixed black spots in the visual field
- mobile bodies as well as a shaded area perceived as a dark curtain.
How long does the retinal detachment surgery take?
The surgery for retinal detachment has a duration that fluctuates between an hour and three hours and is performed under local anesthesia. Surgical therapy is recommended whenever the detachment affects a large area of the retina as well as the central part of the retina (macula).
What not to do with retinal detachment
It is advisable to refrain from physical exertion in the first weeks after retinal detachment surgery. Recovery varies between four and six weeks. Furthermore, recovery times are variable depending on the extent of the detachment and the time elapsed from the event to the time of the surgical insult.
What are the risk factors of retinal detachment?
There are some factors, intrinsic and extrinsic, which can predispose to retinal detachment, among which the most frequent are:
- moderate and severe myopia;
- eye trauma;
- posterior vitreous detachment;
- complication of eye surgery (e.g. cataract surgery);
- inflammatory pathologies (for example, uveitis);
Do you need more information?
Do not hesitate to contact me for any doubt or clarification. I will evaluate your problem and it will be my concern and that of my staff to answer you as quickly as possible.