Index
The concept of "artificial vision" has now lost its science fiction connotation becoming more and more a consolidated reality. The international collaboration between the leading experts in the field of microelectronics, biomaterials, medicine and surgery has in fact already made it possible to recover a certain degree of visual functionality in certain types of patients who have lost their vision in adulthood due to a degenerative retinal disease such as retinitis pigmentosa or age-related macular degeneration.
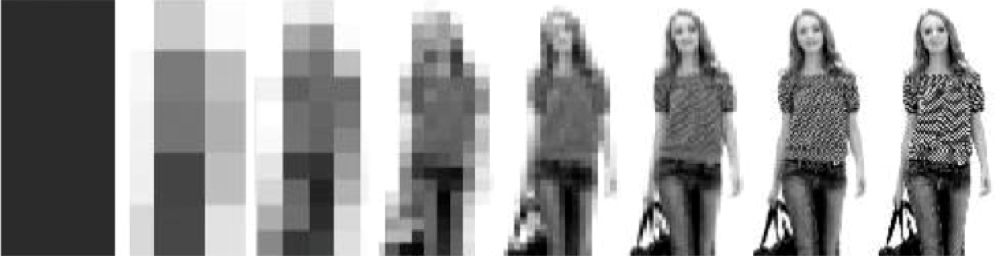
The first retinal prosthesis to receive the CE mark in Europe (2011) and FDA in the United States (2013) was Argus II, produced by the US company Second Sight for visual recovery in blind adult patients suffering from retinitis pigmentosa. It is an epi-retinal prosthesis consisting of a set of microelectrodes mounted on a 4 mm side microchip which is implanted in the vitreous cavity of the eye and fixed in correspondence with the internal retina. Argus II is able to generate a visual perception with a resolution of about 60 pixels thanks to the help of various external components (a video camera mounted on a pair of glasses, a laptop and an external battery) connected to the retinal prosthesis through specific cables which connect the inside of the eye with the outside. The Argus II implant is remarkably invasive and visual recovery rather limited, in fact a perception of luminous dots (phosphenes) is obtained which together create "elementary luminous patterns" which the patient learns to recognize through a specific rehabilitation process able to recognize large elementary geometric figures in white on a black background, letters written in very large characters and in some cases to identify the movement of objects, follow a white line on the floor and find a door.
Despite its criticalities, Argus II represented a milestone in the new era of retinal prostheses, paving the way for the design and construction of several new types of retinal prostheses that are safer and easier to implant and at the same time with a greater number of electrodes and therefore of pixels, to obtain a more detailed visual perception in patients. Allowing patients to recognize faces, move independently in an unfamiliar environment and read complex text is the target towards which researchers in the sector from all over the world are moving.
IRIS II
Other retinal implants that have received the CE mark (2016) include Iris II from the French company Pixium Vision and Alpha AMS from the German company Retina Implant AG.
Iris II is a retinal prosthesis made up of a microchip of 150 micro-electrodes, also designed for visual recovery in patients suffering from retinitis pigmentosa but also Usher syndrome, rod and cone dystrophy and choroideremia. Iris II has similar functionality to Argus II but higher image resolution (150 pixels instead of 60).
Alpha AMS
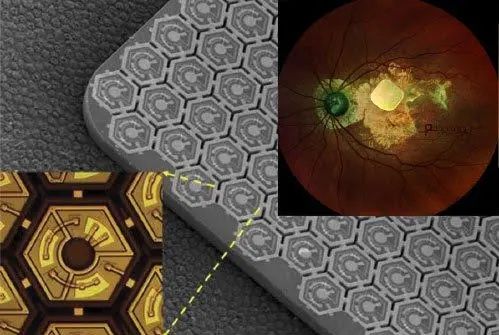
Alpha AMS is a microchip made up of 1600 stimulation units, each made up of a micro-photodiode capable of transforming the light arriving on the retina into an electrical stimulus autonomously, without the aid of external equipment, a signal amplifier and a stimulation micro-electrode. Alpha AMS, unlike Argus II and Iris II, is a sub-retinal prosthesis, which is implanted not in the vitreous cavity but in the sub-retinal space, where it spatially and functionally replaces the photoreceptors.
The retinal prostheses described above have limitations dictated by the invasiveness and complexity of the implant surgery – mainly due to the need to connect the retinal microchip to external elements such as image processors and external batteries – and by the modest visual recovery which does not guarantee recovery of autonomy in daily life. These obstacles seem to be overcome today by the new prosthesis produced by Pixium vision.
First Bionic Vision System
Prima is the first model of retinal prosthesis designed for patients suffering from age-related macular degeneration and is now the subject of a highly anticipated human clinical study to test its applicability and safety.
It is first implanted in the sub-retinal space, in place of the photoreceptors and in contact with the retinal pigment epithelium. The extreme miniaturization and wireless functionality make the Prima implant much less invasive than that of the other prostheses tested to date, in fact no cables are needed anymore coming out of the eye since the images captured and selected by the mini- camera mounted on the patient's glasses are projected onto the prosthesis using near-infrared light and no externally supplied energy is required. The photovoltaic microcells of this prosthesis transform the optical information into electrical stimulation on the bipolar cells of the retina, triggering a visual process very similar to the natural one. Prima's microchip is modular and therefore expandable to increase the width of the field of vision.
The Prima retinal prosthesis can be implanted in patients with end-stage atrophic age-related macular degeneration (geographic atrophy) who have the following characteristics: minimum age 60 years, vision not exceeding 20/400 and absence of foveal perception .
The first implantation of the Prima retinal prosthesis was carried out last December at the Rothschild Foundation in Paris by the surgeon Yannick Le Mer, principal investigator, and with the participation of other illustrious colleagues: Dr. Mahi Muquit, Prof. Jan Van Meurs and Prof. Andrea Cusumano. The microchip was activated 8 weeks after its implantation and the patient was able to perceive the luminous shapes of different objects in the retinal area where light perception was absent.
The speed with which retinal prostheses are evolving gives us hope that in the not too distant future it will be possible to considerably increase the resolution of the images perceived by blind patients who will undergo the implantation of a retinal prosthesis.